Insulin Resistance Uncovered: What Causes It And How To Fix It With Diet
Do you feel exhausted despite getting enough sleep? Struggle to lose stubborn belly fat no matter how much you exercise? Find yourself craving carbs and sugar throughout the day? These frustrating symptoms might not be random—they could be signs that your body isn’t using insulin effectively.
Insulin resistance is a widespread metabolic condition that often goes undiagnosed in its early stages, silently laying the groundwork for more serious health problems. According to the Centers for Disease Control and Prevention (CDC), this condition affects millions of Americans and is a precursor to prediabetes and Type 2 diabetes. What makes insulin resistance so important to understand is that it’s not just about blood sugar—it’s the root cause of numerous chronic conditions that impact health systems worldwide.
In this comprehensive guide, I’ll break down what insulin resistance actually is, the science behind why it happens, how to recognize its symptoms, and most importantly, how dietary changes can be your most powerful tool to address it. You’ll discover why approaches like the carnivore and ketogenic diets are particularly effective strategies to combat insulin resistance at its source.
The good news? Simple changes to what you eat can dramatically improve your body’s response to insulin and transform your health from the inside out.
Table of Contents
What is Insulin Resistance?
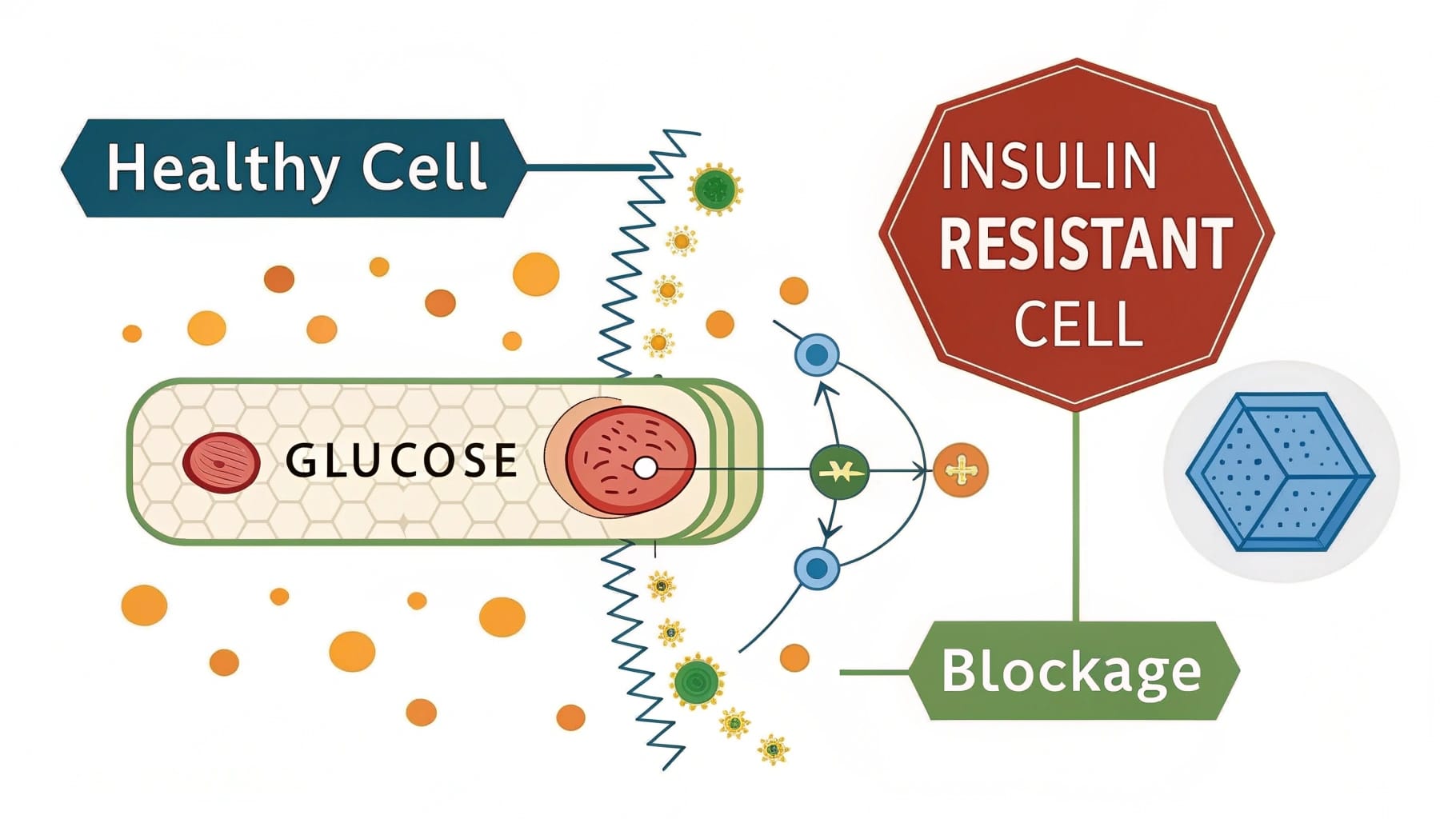
To understand insulin resistance, we first need to grasp how insulin normally functions in a healthy body. Think of insulin as a “key” that unlocks your cells, allowing glucose (blood sugar) to enter and be used for energy or stored for later use. This process is vital for maintaining stable blood sugar levels and providing your body with the energy it needs to function.
When insulin resistance develops, something changes. Your cells’ “locks” begin to malfunction, making the insulin “key” less effective. As a result, your cells become resistant to insulin’s signal, essentially ignoring the hormone’s instruction to take in glucose from the bloodstream.
Your pancreas, detecting high blood sugar levels, responds by producing even more insulin in an attempt to overcome this resistance. This leads to a condition called hyperinsulinemia—abnormally high insulin levels circulating in your bloodstream.
The consequences of this dysfunction are serious: You end up with both elevated blood sugar and high insulin levels, a dangerous combination that sets the stage for metabolic chaos. Your body gets caught in a frustrating cycle: the more insulin it produces, the more resistant your cells become, requiring even more insulin—and on it goes.
Why Does Insulin Resistance Happen? Understanding the Causes & Mechanisms
Insulin resistance doesn’t develop overnight, nor does it have a single cause. Rather, it’s a complex condition influenced by multiple factors that can be broadly categorized into two types: fast-acting mechanisms and slow-developing processes.
Fast Insulin Resistance: The Quick Roadblocks
Some factors can trigger insulin resistance rapidly—within hours or days:
Chronic Hyperinsulinemia: One of the most direct paths to insulin resistance is frequent exposure to high insulin levels, typically from regular consumption of carbohydrate-rich foods. Research published in the Journal of Clinical Investigation shows that when your body experiences too many insulin signals too often, it begins to tune them out—similar to how you might eventually stop noticing a persistent background noise. Studies have demonstrated that insulin resistance can develop remarkably quickly (within days) when subjects are given high-carbohydrate diets or insulin infusions.
Stress Hormones: When you’re stressed, your body releases cortisol and epinephrine (adrenaline), which temporarily raise blood sugar levels as part of your “fight or flight” response. This is actually a survival mechanism designed to ensure you have readily available energy during perceived threats. However, these stress hormones also inhibit insulin signaling, contributing to short-term insulin resistance. When stress becomes chronic rather than occasional, this temporary adaptation becomes a persistent problem.
Acute Inflammation: Inflammatory signals from infections, injuries, or other acute stressors can rapidly disrupt the insulin signaling pathways in your cells, creating a quick onset of insulin resistance that’s usually temporary but can become chronic if the inflammation persists.
Slow Insulin Resistance: The Long-Term Drivers
Over months and years, these factors gradually deteriorate insulin sensitivity:
Adipocyte Hypertrophy (Enlarged Fat Cells): Fat cells have a limit to how much they can expand. When they’re constantly receiving signals to store energy (driven by excess calories and high insulin levels), they grow larger and eventually reach a point where they become resistant to further storage signals. These oversized fat cells also begin releasing harmful inflammatory signals that affect your entire body.
Ectopic Fat Storage: When your primary fat cells become resistant or “full,” excess fatty acids need to go somewhere. Unfortunately, they often end up stored in places where fat doesn’t belong—your liver (causing fatty liver disease), muscles, and even pancreas. This misplaced fat directly causes insulin resistance in those organs, creating a particularly problematic situation when it affects the liver, which plays a crucial role in blood sugar regulation.
Adipose Hypoxia & Chronic Inflammation: As fat cells grow abnormally large, they can outgrow their blood supply, creating areas of low oxygen (hypoxia) within fat tissue. This triggers inflammation within the fat tissue itself that eventually spreads throughout the body. This systemic inflammation further drives chronic insulin resistance in a self-perpetuating cycle.
Ceramides: The Common Mediator
Recent research published in Nature Reviews Endocrinology has identified ceramides—a type of fatty molecule—as a key molecular link in insulin resistance. These ceramides accumulate due to the combined effects of high insulin, inflammation, and excess fat. Once present in cells, they act as specific internal “blocks” that prevent insulin signals from properly activating the cell’s machinery, particularly by interfering with a pathway called AKT that’s essential for insulin function.
Interestingly, studies show that when ceramide production is blocked, insulin sensitivity can be restored even in the presence of other risk factors—suggesting these molecules may be a central mechanism through which various causes ultimately create insulin resistance.
Recognizing the Signs: Common Symptoms of Insulin Resistance
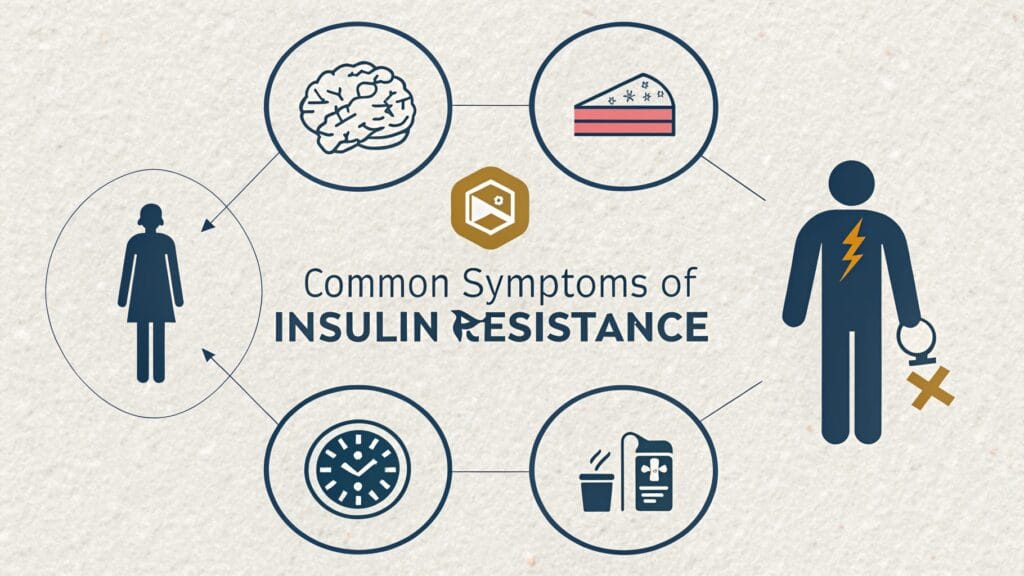
Insulin resistance often develops gradually, with symptoms that might seem unrelated until viewed as part of a larger pattern. Here are the most common signs to watch for:
- Fatigue and low energy (especially after meals)
- Increased hunger and food cravings, particularly for carbohydrates and sugar
- Difficulty losing weight despite diet and exercise efforts
- Increased waist circumference and stubborn belly fat
- Skin tags (small flesh-colored growths on the skin)
- Dark patches of skin (acanthosis nigricans), often on the neck, armpits, or groin
- High blood pressure that develops without other obvious causes
- Abnormal cholesterol and triglycerides (typically high triglycerides and low HDL “good” cholesterol)
- Sleep disturbances including insomnia or sleep apnea
- Brain fog and difficulty concentrating
- Hormonal imbalances (PCOS in women, low testosterone in men)
What makes insulin resistance particularly dangerous is that these symptoms often appear before blood sugar levels rise high enough for a diagnosis of prediabetes or Type 2 diabetes. By the time blood sugar tests become abnormal, insulin resistance has often been present for years, silently damaging your metabolic health.
Why Insulin Resistance Matters: The Gateway to Chronic Disease
Understanding insulin resistance is crucial because it’s not just a symptom—it’s the driving force behind many serious health conditions. Left unaddressed, insulin resistance can progress to:
- Type 2 Diabetes: This is the most direct consequence of longstanding insulin resistance. According to research published in The BMJ, addressing insulin resistance through diet can lead to significant improvements and even medication reduction in Type 2 diabetes patients. Learn more about how diet can reverse Type 2 diabetes.
- Prediabetes: The intermediate stage between healthy metabolism and Type 2 diabetes, characterized by blood sugar levels that are elevated but not yet in the diabetic range.
- Non-Alcoholic Fatty Liver Disease (NAFLD): Excess fat accumulation in the liver, which can progress to inflammation and even liver fibrosis if not addressed.
- Polycystic Ovary Syndrome (PCOS): A hormonal disorder common among women of reproductive age, with insulin resistance as a key underlying factor.
- Cardiovascular Disease: Insulin resistance contributes to atherosclerosis, heart disease, and stroke risk through multiple mechanisms including inflammation, hypertension, and dyslipidemia.
- Certain Cancers: Research increasingly links insulin resistance to higher risk of several cancer types, including breast, colon, and pancreatic cancers.
- Alzheimer’s Disease: Sometimes called “Type 3 Diabetes” due to the role of insulin resistance in brain tissue, as described in research from the Journal of Diabetes Science and Technology, contributing to cognitive decline.
- Other Conditions: Hypertension, dyslipidemia, gout, and numerous other metabolic disorders have strong connections to insulin resistance.
Understanding the wide-ranging impacts of insulin resistance reveals why addressing it should be a priority for anyone concerned with long-term health and disease prevention.

How Diet is Your Most Powerful Tool Against Insulin Resistance
When it comes to combating insulin resistance, multiple lifestyle factors play important roles—exercise, quality sleep, and stress management all contribute to improved insulin sensitivity. However, diet stands out as the most powerful and direct lever for change because it directly influences the key drivers: blood sugar and insulin levels.
The core principle is straightforward: reducing the dietary demand for insulin allows sensitivity to gradually return. While your body is constantly exposed to high insulin levels (driven primarily by carbohydrate intake), the cellular resistance persists and often worsens. By dramatically reducing this insulin stimulus, you give your cells a chance to reset and regain their normal responsiveness.
This is why Low-Carbohydrate Ketogenic Diets (LCKD) have proven exceptionally effective for improving insulin sensitivity. By minimizing carbohydrate intake, you prevent the glucose spikes that trigger insulin release, effectively lowering both blood sugar and insulin levels. This breaks the cycle of hyperinsulinemia that drives fast insulin resistance and, over time, allows the slower mechanisms to improve as well.
Clinical studies on low-carb ketogenic diets, like one published in Nutrition & Metabolism showing significant improvements in Type 2 Diabetes markers, demonstrate the real-world power of this dietary approach in combating insulin resistance. Research from the American Diabetes Association further confirms that many patients see substantial improvements in blood glucose control, with some able to reduce or eliminate medications under proper medical supervision.
The Carnivore Diet: A Targeted Strategy for Improving Insulin Sensitivity
Within the spectrum of low-carbohydrate approaches, the carnivore diet represents perhaps the most targeted strategy for addressing insulin resistance, working directly on multiple mechanisms we’ve discussed.
Here’s why carnivore eating is particularly effective for improving insulin sensitivity:
Near-Zero Carbohydrates: The carnivore diet essentially eliminates carbohydrates entirely, focusing on animal protein and fats. This maximally reduces glucose and insulin spikes, directly addressing the fast insulin resistance mechanism of hyperinsulinemia. With virtually no dietary carbohydrate intake, insulin levels remain consistently low, allowing cellular sensitivity to gradually restore.
Focus on Nutrient-Dense Animal Foods: Animal-based foods provide essential nutrients without the plant compounds that can be inflammatory for some individuals. This anti-inflammatory effect can help reduce one of the key drivers of insulin resistance, particularly for those with sensitivities to certain plant foods.
Natural Calorie Regulation: Protein and fat are exceptionally satiating, as confirmed by research in The American Journal of Clinical Nutrition, which often leads to naturally reduced calorie intake without conscious restriction. This supports weight loss and particularly the reduction of visceral fat (the dangerous fat around organs), helping address the adipocyte hypertrophy and ectopic fat storage that drive slow insulin resistance.
Metabolic State: The carnivore diet promotes a state of nutritional ketosis, where your body primarily burns fat for fuel rather than glucose. This metabolic shift is virtually impossible to achieve when insulin levels are chronically elevated, but becomes accessible when insulin drops—creating a virtuous cycle that further improves insulin sensitivity.
What makes the carnivore approach uniquely powerful is that it’s essentially a simplified, intensified form of a low-carb ketogenic diet that addresses multiple root causes identified in insulin resistance research. Many people who struggle with more moderate low-carb approaches find that the clarity and simplicity of carnivore eating makes it easier to maintain consistently, which is crucial for long-term metabolic healing.
Testing for Insulin Resistance: Knowing Your Numbers
If you suspect insulin resistance might be affecting your health, several lab tests can help confirm your status and track improvements:
Fasting Glucose: This basic blood sugar test measures glucose levels after at least 8 hours without food. While normal ranges are typically listed as 70-99 mg/dL, optimal levels for metabolic health may be closer to 70-85 mg/dL.
Fasting Insulin: This critical test directly measures insulin levels and is often overlooked in standard medical testing. Optimal fasting insulin is generally below 5 μIU/mL, with levels above 10 μIU/mL suggesting significant insulin resistance even when blood sugar appears normal.
HbA1c (Glycated Hemoglobin): This test provides an average of blood sugar levels over the previous 2-3 months. Normal ranges are typically listed as below 5.7%, with 5.7-6.4% indicating prediabetes and 6.5% or higher suggesting diabetes. For optimal metabolic health, many experts suggest targeting levels below 5.4%.
HOMA-IR (Homeostatic Model Assessment of Insulin Resistance): This calculation uses both fasting glucose and insulin to provide a more comprehensive assessment of insulin resistance. The formula is: (Fasting Insulin × Fasting Glucose) ÷ 405. Scores below 1.0 indicate optimal insulin sensitivity, 1.0-2.0 suggest moderate insulin resistance, and above 2.0 indicate significant insulin resistance.
Triglyceride/HDL Ratio: This simple calculation from a standard lipid panel correlates strongly with insulin resistance. Divide your triglyceride level by your HDL cholesterol. Ratios below 2.0 are optimal, while ratios above 3.0 suggest insulin resistance.
While at-home glucose monitors can provide useful information about how specific foods affect your blood sugar, laboratory testing provides the most comprehensive assessment. Consider working with a healthcare provider knowledgeable about metabolic health to interpret your results and track improvements over time.
Taking Action: Practical Steps to Improve Insulin Sensitivity
Now that we understand the mechanisms of insulin resistance and its importance to overall health, let’s focus on practical steps to improve insulin sensitivity:
Prioritize Dietary Change: The single most effective intervention is drastically reducing carbohydrate intake. Following a carnivore or ketogenic approach means focusing on quality animal proteins and fats while eliminating or severely restricting carbohydrates. This strategy targets insulin resistance at its source by minimizing insulin secretion.
- When starting out, focus more on what to limit (carbohydrates) rather than how much to eat (calorie restriction). Many people naturally regulate their intake on these diets without counting calories.
- Emphasize fatty cuts of meat, eggs, and other animal products that provide both protein and healthy fats.
- Be particularly cautious with hidden sources of sugar and refined carbohydrates that can trigger insulin spikes.
Incorporate Regular Movement: Exercise improves insulin sensitivity through multiple mechanisms, according to Mayo Clinic research. Both strength training and cardiovascular activity are beneficial, with studies published in the Journal of Physiology suggesting that high-intensity interval training (HIIT) may be particularly effective for metabolic health.
Manage Stress: Chronic stress contributes to insulin resistance through elevated cortisol levels. Incorporating stress management practices like meditation, deep breathing exercises, time in nature, or engaging in fulfilling hobbies can help mitigate this effect.
Prioritize Quality Sleep: Poor sleep directly impacts insulin sensitivity. Aim for 7-8 hours of quality sleep in a cool, dark room, and consider establishing a consistent sleep schedule.
MEDICAL DISCLAIMER
This information is provided for educational purposes only and is not intended as medical advice. Always consult with a qualified healthcare provider BEFORE making significant dietary changes or starting any new health regimen, especially if you have a medical condition or take medications.
Importantly, if you’re currently taking medication for diabetes or blood pressure, dietary changes can significantly alter your body’s needs for these medications. Medical supervision is essential to safely monitor and adjust dosages as your metabolic health improves.
Conclusion: Taking Control of Your Metabolic Health
Insulin resistance is an incredibly common but addressable metabolic condition that affects millions of people, often without their knowledge. Understanding how insulin resistance develops—through both fast mechanisms like hyperinsulinemia and slow processes like abnormal fat storage and inflammation—is the first step toward reclaiming your metabolic health.
The power of dietary interventions, particularly low-carbohydrate approaches like carnivore and ketogenic diets, lies in their ability to directly target the root causes of insulin resistance rather than just managing symptoms. By dramatically reducing the insulin demand on your body, these nutrition strategies create an environment where your natural insulin sensitivity can gradually return.
Remember that metabolic healing takes time. The same mechanisms that slowly developed over years will also take time to reverse. However, many people report noticeable improvements in energy, weight management, and other symptoms within weeks of making these dietary changes.
The journey to metabolic health is personal, but you are not alone. Armed with an understanding of insulin resistance and effective tools to combat it, you have the power to transform your health from the inside out.
Your Next Steps
Have you experienced symptoms of insulin resistance? Are you currently following a carnivore or keto approach to improve your metabolic health? I’d love to hear about your experiences in the comments below.
If you’re ready to take action against insulin resistance, check out these resources to support your journey:
- How diet led to medication reduction in a scientific study on Type 2 Diabetes
- What is Keto Flu? Understanding Symptoms and Causes
- Carnivore Diet Food List: What to Eat and Avoid
- Combining Intermittent Fasting with Keto and Carnivore Diets
- Practical Carnivore Diet Meal Ideas to Get Started
- Essential Electrolytes on the Carnivore Diet
Remember to share this article with friends or family members who might benefit from understanding insulin resistance and how dietary changes can help address it.
Your metabolic health journey is one of the most important investments you can make in your long-term wellbeing—and it starts with understanding the science behind insulin resistance.
Enjoy, Review – We Value Your Opinion!
There are no reviews yet. Be the first one to write one.